Scientists have successfully restored the lost uricase enzyme, a key breakthrough in combating fructose-induced fat formation. This discovery offers new hope for preventing obesity and metabolic disorders by targeting how the body processes sugar and stores fat.
Limited Quantities Available! Order Today and Enjoy Free Shipping on Orders Over $100!
Whitepaper Series: The Fructose Model — The Metabolic Energy Failure Framework
Updated at:

Executive Summary
Thesis: Across chronic disease, a recurring early signature appears: cellular energy failure. Many stressors can cause it — infection, toxins, hypoxia, inflammation — but the most universal and modifiable amplifier is fructose metabolism, specifically phosphorylation by fructokinase (KHK) [MECH-M1993] [MECH-N2005].
Mechanism: Fructose metabolism directly creates this state by bypassing normal metabolic checkpoints. Rapid phosphorylation by fructokinase burns through ATP in a single step, generating uric acid and reactive oxygen species that suppress mitochondria, reduce nitric oxide, and trigger inflammation. The result is a predictable low-energy pattern — a conservation program useful in scarcity, harmful in chronic excess [CORE-RSTB2023].
Triggers:
- External: sugars, HFCS, alcohol
- Internal: the polyol pathway, triggered by high glucose, salt/osmolality, dehydration, hypoxia, or stress [ENDO-L2013] [ENDO-AH2021].
Because these inputs are redundant, restriction alone rarely holds. The modern food environment keeps the switch engaged continuously.
Perspective: The problem is not fructose’s existence, but its persistence. In nature, activation was brief and cyclical; today it is constant. Over time, excess and duration turn a survival tool into an amplifier of dysfunction.
Implication: If fragile, energy-starved cells are the common early stage of chronic disease — and fructose metabolism reproducibly amplifies that state — then testing and falsifying this model becomes critical. It offers a single, measurable hypothesis for why diverse diseases share the same low-energy signature, and why that signature has intensified alongside continuous sugar availability, refined carbohydrates, and processed foods. Understanding when this switch became chronically engaged may clarify not only how disease develops, but why the modern metabolic crisis emerged.
Seen through this lens, excess fructose metabolism is the leak in metabolic health — one that persists despite decades of downstream repair. Modulating this pathway may not be another treatment layer, but an upstream fix: sealing the leak, not mopping the floor.
Integration: The result is a coherent map from fragile cells → fragile systems: metabolic syndrome, vascular dysfunction, neurodegeneration, and even cancer’s glycolytic bias can be understood as expressions of chronic low-energy biology [MECH-J2007]. This framework does not replace other models; it unifies them. Calories, insulin, lipids, and inflammation still matter — but they converge downstream of the same low-energy switch, explaining why so many chronic diseases move in parallel.
Open Science DeclarationThis framework is offered as an open, falsifiable hypothesis — not a proprietary claim — and we acknowledge the potential for bias whenever new ideas emerge from those who propose them. Our goal is to democratize the model and its potential modulators so that scientists, clinicians, and citizen researchers can test, challenge, and refine it in the open. An appendix will outline testable protocols that any institution can adopt to add value to the model without asserting ownership or agenda. Whether the data confirm or refute it, the outcome is equally meaningful. Validation would strengthen the case for prevention over repair; falsification would still be a breakthrough, ruling out what appears to be the most evidence-based universal amplifier of chronic disease. Either result advances the same aim: shifting medicine’s focus from managing damage to understanding cause — and, ultimately, restoring metabolic health at its source. |
1. Mechanism & Biochemistry of Fructose Metabolism
This section reviews how fructose metabolism uniquely drives ATP depletion and mitochondrial suppression.
Fructose metabolism bypasses the body's normal checkpoints. Once inside the cell, it is rapidly phosphorylated by fructokinase, consuming ATP in a single burst. This energy drop generates uric acid, increases oxidative stress, and reduces nitric oxide, which constrains blood flow and energy delivery [MECH-N2005].
The mitochondria—the cell's engines—shift down to conserve fuel. The body interprets this as scarcity: metabolism slows, hunger rises, and fat is stored. This cascade is clear, reproducible, and uniquely tied to fructose metabolism.
[Read the full Mechanism Whitepaper →]
2. Fragile Cells → Fragile Systems
This section explores how energy-starved cells accumulate into systemic dysfunction.
When cells run chronically in eco-mode, they become fragile. Imagine the city's mail trucks: if one breaks down, deliveries continue. But if the entire fleet shares the same engine failure, the system collapses.
In biology, fragile cells accumulate into fragile organs and fragile systems. Hypertension, diabetes, fatty liver, even Alzheimer's are not separate origins, but manifestations of fragile, energy-starved systems. Micro-failures at the cellular level scale into macro-failures across the body.
[Read the Fragile Systems Whitepaper →]
3. Endogenous Fructose Production
This section describes how the body makes its own fructose through the polyol pathway.
Fructose is not just something we eat. Through the polyol pathway, the body makes it internally, converting glucose into sorbitol and then fructose. This occurs in response to high glycemic loads, salt, dehydration, alcohol, hypoxia, and stress [ENDO-L2013].
This discovery explains why metabolic disease can persist even in people who avoid added sugar. It also helps resolve decades of debate around "healthy" food choices—why two people can eat differently yet arrive at similar health outcomes.
Many of the arguments over carbs, salt, alcohol, or even stress management are actually arguments about different triggers of the same pathway. What once seemed contradictory now unifies into one upstream mechanism.
[Read the Endogenous Fructose Whitepaper →]
4. Fat Gain as a Natural Consequence
This section reframes fat gain as an intended output of the survival program.
Fructose metabolism is not a mistake—it's an energy management program. In times of surplus, the trigger allows us to take advantage of abundance, converting extra fuel into stored fat. In times of scarcity, the same trigger conserves resources, slowing metabolism to preserve energy for survival [NAT-J2020].
This means fat gain is only half the story. The same mechanism also explains why fatigue sets in, why cravings persist, and why the brain feels starved even when the body has fuel. It is not just about storing energy—it is about reshaping our entire physiology around conservation.
[Read the Fat Gain Models Whitepaper →]
5. The Burden of Evidence
5.1 Lessons from Nature
Fructose metabolism is found across species as a survival tool. Bears fatten before hibernation; birds conserve water during migration; desert mammals and naked mole rats rely on it for dehydration and hypoxia tolerance [NAT-P2017].
In humans, the same system now runs year-round. A tool designed for survival has become a chronic liability.
[Read the Nature’s Playbook Whitepaper →]
5.2 The Fruit Paradox
Fruit is not the problem—it is the perfect example of this system working as designed. Unripe fruit protects seeds with polyphenols; ripe fruit shifts toward fructose to attract animals; fermentation signals scarcity through alcohol. Each phase maps to the same biochemical arc: protection, attraction, urgency [NAT-D2004].
[Read the Fruit & Fructose Whitepaper →]
5.3 Historical Context
For most of history, sugar was scarce. Gout and obesity were confined to elites. Industrialization made fructose cheap and constant, aligning with the surge in metabolic disease [HIST-Y1972].
[Read the Historical Evidence Whitepaper →]
6. From Energy Failure to Disease: The Four Horsemen
This section examines how fructose metabolism manifests across major disease categories.
6.1 Metabolic Dysfunction
Obesity, type 2 diabetes, fatty liver disease, and gout all emerge directly from chronic fructose metabolism. Fat storage, insulin resistance, and uric acid production are not side effects—they are the intended outputs of the program running in overdrive [DIS-J2013].
[Read the Metabolic Dysfunction Whitepaper →]
6.2 Cardiovascular Disease
Fructose metabolism generates uric acid and oxidative stress, which impair nitric oxide and stiffen blood vessels. This drives hypertension and vascular dysfunction—the earliest footprints of cardiovascular disease. Over time, fragile vessel systems manifest as heart attacks, strokes, and heart failure [CVD-F2008].
[Read the Cardiovascular Whitepaper →]
6.3 Neurodegeneration
The brain is especially vulnerable to energy failure. Endogenous fructose production in neurons drives insulin resistance, lowering ATP and impairing memory circuits—mapping onto the “type 3 diabetes” concept in Alzheimer’s and related disorders [NEURO-J2020].
[Read the Neurodegeneration Whitepaper →]
6.4 Cancer
Tumor cells favor low-oxygen, glycolytic conditions. Fructose metabolism promotes this state by depleting ATP, generating uric acid, and suppressing mitochondria—creating fertile metabolic ground for growth and survival under stress [CANC-N2020].
[Read the Cancer Whitepaper →]
7. Intervention Strategies
This section highlights strategies that converge on fructose metabolism as the common pathway.
For decades, health guidance has emphasized diet, exercise, hydration, and lifestyle. Each works—because each lowers fructose exposure or reduces endogenous triggers.
But restrictive diets fail at scale because the body has multiple redundant ways of producing fructose internally.
A key clue comes from a rare condition called essential fructosuria. Individuals born without a functioning fructokinase enzyme simply excrete fructose harmlessly—and do not develop metabolic disease. This suggests that the most promising course of intervention is not endless restriction, but directly targeting the pathway itself [INT-EF2009].
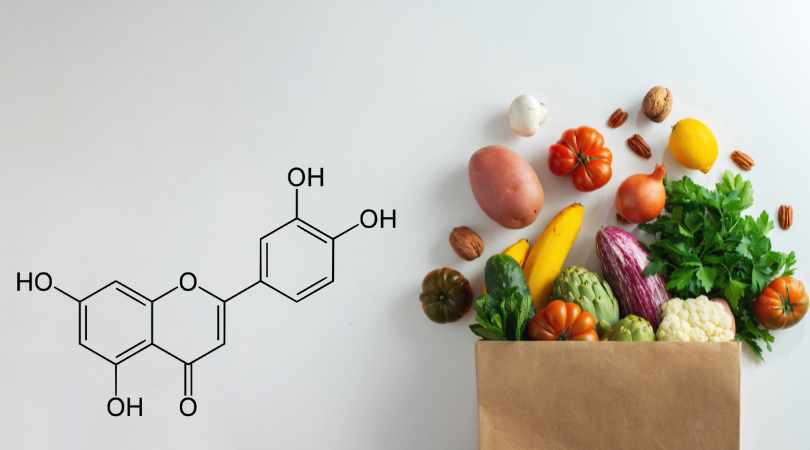
Emerging strategies include lifestyle measures, hydration and salt management, nutraceuticals like luteolin, and pharmaceutical inhibitors of fructokinase. These are not replacements for standard care, but complements—reinforcing the foundation so that existing treatments have a better chance of success and a durable conclusion [INT-LE2016] [INT-S2023].
[Read the Interventions & Future Research Whitepaper →]
Conclusion
The Metabolic Energy Failure Framework unites fragmented theories of chronic disease under one testable model. Fragile cells become fragile systems, and fructose metabolism is the upstream switch that sets the stage.
By draining ATP, generating uric acid, and suppressing mitochondria, fructose metabolism triggers the full metabolic dysfunction signature:
- Insulin resistance
- Chronic inflammation
- Hormonal disruption (leptin, ghrelin, stress hormones)
- Cravings and appetite dysregulation
- Fat storage and weight gain
- Systemic fatigue and organ fragility
And critically, it functions as a loop. Energy depletion signals hunger → hunger drives intake → intake deepens energy depletion. In today's food environment, where sugar is abundant, this loop never resets. A survival switch designed for scarcity has become a trap of abundance.
Understanding and modulating this pathway allows us to move beyond symptom management toward restoring cellular performance. This is not just about longer life, but better life—built on energy, clarity, and resilience.
These relationships form a coherent, testable framework to be addressed in a forthcoming appendix with a falsifiable research protocol.
(Selected keystone sources linked inline; full citations in the Master Bibliography.)
Disclaimer: The information in this blog reflects personal opinions, experiences, and emerging research. It is not intended as medical or professional advice and should not replace consultation with qualified professionals. The accuracy of this content is not guaranteed. Always seek guidance from a licensed expert before making any health-related decisions.