Scientists have successfully restored the lost uricase enzyme, a key breakthrough in combating fructose-induced fat formation. This discovery offers new hope for preventing obesity and metabolic disorders by targeting how the body processes sugar and stores fat.
Limited Quantities Available! Order Today and Enjoy Free Shipping on Orders Over $100!
6.2 Cardiovascular Disease: Fragile Vessels from Fragile Energy
Updated at:

Abstract
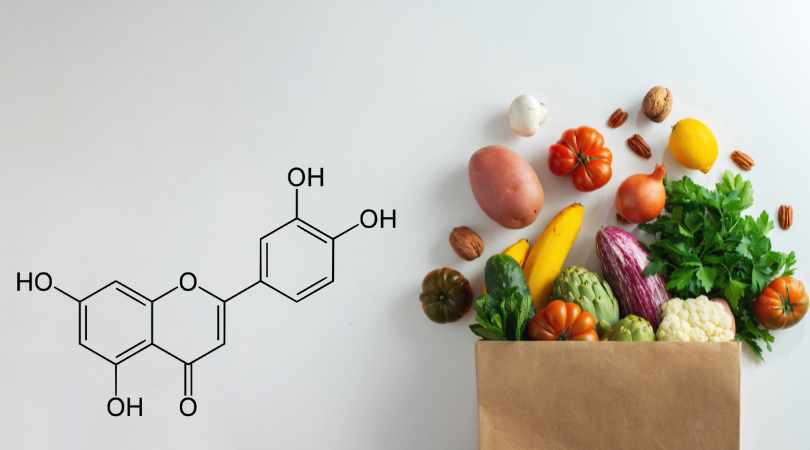
Cardiovascular disease (CVD) remains the leading global cause of death. Traditional risk factors — salt, obesity, and cholesterol — have been treated as independent variables, but all converge on a deeper upstream mechanism: fructose metabolism. Fructose rapidly consumes ATP, generating uric acid and oxidative stress that reduce nitric oxide (NO), the molecule that keeps blood vessels flexible. As NO falls, vessels stiffen, pressure rises, and energy-starved endothelial cells give way to fragile vasculature. Fragile cells become fragile vessels — and fragile vessels, fragile systems [CORE-RSTB2023].
1. Introduction: The Burden of Fragile Vessels
Cardiovascular disease accounts for roughly one-third of global deaths. It is often described as a disease of excess — of salt, cholesterol, or inactivity. Yet these surface risks mask a deeper biochemical unity: all activate or amplify fructose metabolism. Whether ingested directly (sugar, HFCS, alcohol, fruit juice) or generated internally (via glucose spikes, salt/osmolality, dehydration, or hypoxia), fructose metabolism drains ATP, produces uric acid, and weakens vascular resilience [MECH-J2007].
2. Mechanism: How Fructose Weakens the Vascular System
2.1 ATP depletion and uric acid generation
Fructokinase (KHK) phosphorylates fructose rapidly, consuming ATP and yielding uric acid as a byproduct. Endothelial cells — thin and metabolically active — are among the first to experience this energy drop. Intracellular uric acid amplifies oxidative stress, promoting vascular inflammation and endothelial dysfunction [CVD-KA2005] [CVD-ZH2008].
2.2 Oxidative stress and nitric oxide loss
Uric acid and reactive oxygen species (ROS) scavenge NO, the vasodilator responsible for arterial elasticity and blood flow. The resulting loss of NO stiffens vessels, raises blood pressure, and links vascular dysfunction with insulin resistance [CVD-K2005] [CVD-F2008].
2.3 From micro to macro fragility
Energy-depleted endothelial cells become fragile and inflamed. Over time, this fragility scales up: from cell → vessel → organ → system. The earliest manifestation is hypertension; the endpoint is multi-system cardiovascular fragility.
2.4 The renal axis: pressure that “sticks”
In the kidney, fructose metabolism in proximal tubules increases sodium reabsorption and impairs nitric oxide signaling. The result is salt-sensitive hypertension, even with moderate sodium intake. Fructose metabolism therefore integrates vascular and renal mechanisms of blood pressure regulation [CVD-N2006].
2.5 Lipid linkage: hepatic fructose → vascular injury
Fructose metabolism in the liver accelerates de novo lipogenesis (DNL), raising VLDL and triglycerides. These lipids penetrate a damaged endothelium, fostering atherosclerotic plaque. Cholesterol remains relevant — but fructose creates the biochemical conditions that make cholesterol harmful [MECH-S2019].
3. Hypertension: The First Footprint
Hypertension often appears first in the cascade of vascular fragility.
- Salt: High sodium raises plasma osmolality, activating endogenous fructose production. The resulting uric acid suppresses NO, stiffening vessels and raising pressure [ENDO-AH2021].
- Obesity: Promotes dehydration, insulin resistance, and salt retention — all fructose-activating triggers.
- Sugar: Beverages high in fructose acutely raise blood pressure in both animals and humans [CVD-B2008] [CVD-PP2010].
These inputs are not separate culprits — they are multiple entry points into the same biochemical pathway.
4. Potassium: The Missing Half of “Salt”
Modern diets favor sodium and neglect potassium, altering vascular physiology. Low potassium impairs NO synthesis, enhances vasoconstriction, and promotes renal sodium retention. A balanced Na⁺:K⁺ ratio mitigates osmolality stress, reduces endogenous fructose signaling, and supports vascular health [DIS-J2013].
5. Atherosclerosis and Vascular Dysfunction
Once hypertension and oxidative stress set in, the vascular lining progressively fails:
- Oxidative stress and inflammation damage the endothelium.
- Insulin resistance in vascular tissue impairs NO production and promotes smooth muscle proliferation.
- Glycocalyx thinning exposes the endothelium to further mechanical and metabolic damage.
Fructose metabolism, by lowering ATP and elevating uric acid, supplies the common upstream thread linking vascular stiffening, plaque formation, and ischemia.
6. Clinical Evidence and Reversibility
- Experimental data: Fructose-fed animals consistently develop hypertension and vascular stiffness; blocking uric acid restores NO and normalizes blood pressure [CVD-N2006].
- Human data: Uric acid–lowering with allopurinol significantly lowers BP in adolescents with early hypertension [CVD-FJ2008].
- Acute studies: Single fructose loads transiently elevate BP even in healthy adults, confirming the direct hemodynamic effect [CVD-B2008].
These findings demonstrate not only correlation but causality — fructose metabolism itself alters vascular tone, oxidative balance, and renal handling of salt and uric acid.
7. Conclusion
Cardiovascular disease can be reinterpreted as the natural endpoint of vascular energy failure. Fructose metabolism creates the triad of ATP depletion, uric acid elevation, and nitric oxide loss that drives hypertension, atherosclerosis, and heart failure. Cholesterol, salt, and obesity are not competing hypotheses — they are expressions of the same conserved biochemical program for survival under scarcity. In the modern world of constant abundance, that program becomes destructive.
These relationships form a coherent, testable framework to be addressed in forthcoming experimental protocols.
(Selected sources linked inline; full citations in the Master Bibliography.)
Disclaimer: The information in this blog reflects personal opinions, experiences, and emerging research. It is not intended as medical or professional advice and should not replace consultation with qualified professionals. The accuracy of this content is not guaranteed. Always seek guidance from a licensed expert before making any health-related decisions.