Scientists have successfully restored the lost uricase enzyme, a key breakthrough in combating fructose-induced fat formation. This discovery offers new hope for preventing obesity and metabolic disorders by targeting how the body processes sugar and stores fat.
Limited Quantities Available! Order Today and Enjoy Free Shipping on Orders Over $100!
7.0 Intervention Strategies: Turning Down the Survival Switch
Updated at:

Abstract
Most public health strategies against metabolic disease have focused on restriction — eat less, avoid sugar, exercise more. Yet despite decades of effort, obesity, diabetes, fatty liver, and hypertension have surged worldwide. The Fructose Model offers a new explanation: these conditions stem from an overactive survival program built around fructose metabolism. Even without added sugar, the body produces fructose internally through the polyol pathway, triggered by high glucose, salt, dehydration, alcohol, and hypoxia. Restriction alone cannot silence this program; intervention must act upstream to modulate it directly [CORE-RSTB2023].
1. Why Restriction Alone Fails
1.1 A biological driver shared by all animals
Fructose metabolism is not a flaw — it is a survival adaptation shared across species. Sweet, salty, and umami tastes activate conserved biochemical pathways that promote fat storage and water retention during scarcity. Asking humans to override these drives indefinitely is unrealistic; biology always wins.
1.2 Redundant reinforcement
- Even with zero added sugar, the polyol pathway converts glucose to fructose inside the body [ENDO-L2013].
- Salt, dehydration, alcohol, and hypoxia activate the same pathway [ENDO-AH2021].
- Obesity itself feeds the cycle through higher osmolality, sleep apnea, and systemic stress.
1.3 The problem of restrictive diets
Dieting fails for biological and social reasons. Abstinence increases cravings, fatigue, and mood instability — symptoms fueled by the very pathway being targeted. Restriction fights against survival circuitry, leading to frustration, relapse, and guilt. The unifying truth: restriction cannot overcome biology at scale.
2. Lessons from Essential Fructosuria
Essential fructosuria is a benign genetic condition in which individuals lack fructokinase (KHK-C). They excrete fructose harmlessly in urine and remain protected from metabolic syndrome. This natural experiment reveals:
- Fructokinase (KHK-C) is the master switch. Without it, fructose cannot activate the survival program [INT-EF1994].
- The pathway is optional. Its absence does not harm health [INT-EF2003].
- It blocks both dietary and endogenous fructose. By removing the entry enzyme, ATP depletion and uric acid formation are prevented at the source [INT-EF2009].
Essential fructosuria thus proves that targeting KHK can safely “turn off” the program without adverse effects — an ideal intervention point.
3. Reinforcing the Foundation: Lifestyle and Nutrition
3.1 Reduce exogenous fructose
Eliminating added sugars, HFCS, and sugary drinks reduces load. Whole fruit remains buffered by fiber and water, but juicing and drying strip these protections [MECH-T2010].
3.2 Moderate high-glycemic carbohydrates
Stabilizing glucose prevents polyol activation and smooths insulin signaling, reducing both exogenous and endogenous fructose formation.
3.3 Balance salt, potassium, and hydration
Modern diets are sodium-rich and potassium-poor, which raises osmolality and stimulates endogenous fructose production. Proper hydration and potassium intake counteract this signal [ENDO-AH2021].
3.4 Alcohol moderation
Alcohol metabolism overlaps with fructose, generating uric acid and oxidative stress. In ancestral settings, alcohol was rare and seasonal; today it is constant, keeping the pathway chronically engaged [NAT-D2004].
3.5 Improve sleep and oxygenation
Sleep apnea and chronic hypoxia activate the same energy-conservation pathway that fructose triggers. Treating these improves both brain and systemic energy metabolism [ENDO-P2017].
3.6 Physical activity
Exercise increases mitochondrial density and nitric oxide (NO), directly countering fructose-induced suppression and vascular stiffness [CVD-F2008].
4. Direct Modulation of the Pathway
4.1 Pharmaceutical KHK inhibitors
Clinical trials confirmed that KHK inhibition improves liver fat, insulin resistance, and uric acid levels:
- PF-06835919: Reduced hepatic fat and uric acid in phase 2 trials [INT-S2023].
- LY3522348: First-in-human data confirming safety and engagement [INT-F2025].
- Preclinical work: KHK deletion protected against NASH and kidney injury [INT-SH2020] [INT-AH2017].
4.2 Nutraceutical modulators
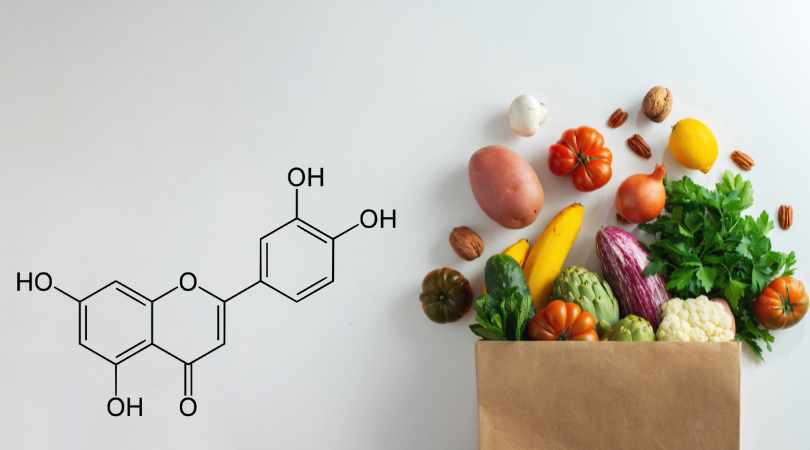
Luteolin is the most validated natural KHK inhibitor:
- Identified through bioactivity-guided screening [INT-LE2016].
- Improves insulin sensitivity, reduces liver fat, lowers blood pressure, and protects neurons.
- Liposomal delivery resolves poor bioavailability and enhances systemic reach.
- RCTs with artichoke + luteolin (Altilix®) confirm improved liver fat, insulin resistance, and visceral adiposity [INT-ALT2019] [INT-ALT2023].
Other natural compounds under study include:
- Osthole — reduces cardiac fructokinase activity and oxidative stress [INT-OST2023].
- D-Mannose — potential competitive substrate; limited data but mechanistically plausible.
4.3 Uric acid reduction
Since uric acid amplifies the fructose response, lowering it offers synergy:
- Pharmaceuticals: allopurinol, febuxostat.
- Nutraceuticals: tart cherry extract, quercetin.
These lower oxidative stress and vascular stiffness but should complement — not replace — KHK modulation [INT-J2023].
5. Energy Failure as the Root Disease
Modern medicine treats symptoms — insulin resistance, high cholesterol, inflammation — rather than the underlying cause. The Fructose Model reframes these as secondary expressions of a deeper lesion: cellular energy failure. Targeting fructose metabolism strengthens all other therapies by addressing the foundation itself. Clinical data show that sugar restriction or KHK inhibition can rapidly normalize liver fat and insulin sensitivity, often within weeks [INT-SCHW2017].
6. The Future of Intervention
Our environment ensures constant activation of the fructose pathway. The goal is not denial but modulation — turning down the switch. Combining lifestyle improvements with direct pathway inhibition restores energy stability and appetite control, allowing behavior change to sustain itself. When applied at scale, this approach could reduce multiple chronic diseases simultaneously.
7. Conclusion
The Fructose Model reframes chronic disease as a single problem — energy failure — with diverse symptoms. Restriction alone cannot fix it. But by targeting the master enzyme, fructokinase, and modulating its downstream amplifiers like uric acid, we can stabilize metabolism at its root.
Luteolin stands out as the leading natural candidate for safe, broad-based pathway modulation. Inhibiting fructose metabolism does not fight biology; it restores balance to it — turning off the survival switch that no longer serves its purpose in an age of excess.
These relationships form a coherent, testable framework to be addressed in forthcoming experimental protocols.
(Selected sources linked inline; full citations in the Master Bibliography.)
Disclaimer: The information in this blog reflects personal opinions, experiences, and emerging research. It is not intended as medical or professional advice and should not replace consultation with qualified professionals. The accuracy of this content is not guaranteed. Always seek guidance from a licensed expert before making any health-related decisions.