Scientists have successfully restored the lost uricase enzyme, a key breakthrough in combating fructose-induced fat formation. This discovery offers new hope for preventing obesity and metabolic disorders by targeting how the body processes sugar and stores fat.
Limited Quantities Available! Order Today and Enjoy Free Shipping on Orders Over $100!
Fatty Liver
A condition where fat accumulates in the liver, often driven by fructose metabolism—can lead to inflammation and insulin resistance.
A Silent Epidemic Begins in the Liver
Fatty liver isn’t just about eating fat—it’s often about how your body handles sugar, especially fructose.
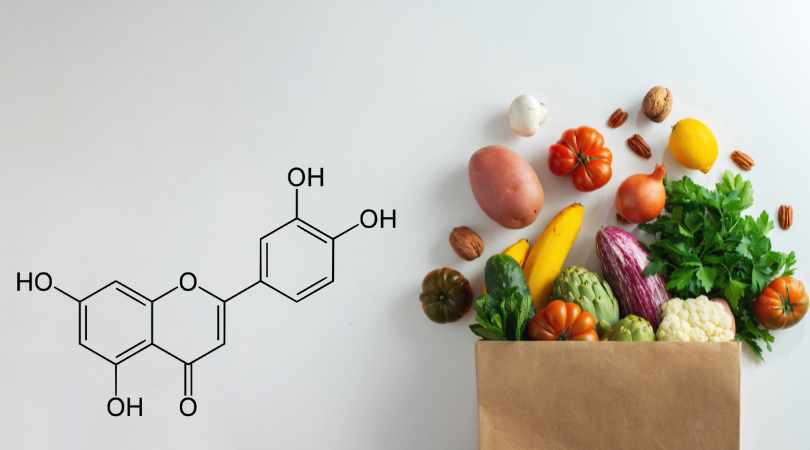
Fructose is uniquely lipogenic, meaning it turns into fat more efficiently than other sugars—directly in the liver. This fat buildup can occur even in lean individuals, especially when endogenous fructose is produced under stress or high-carb intake, silently progressing into non-alcoholic fatty liver disease (NAFLD).
SugarShield is designed to support metabolic health at the root. By helping manage the effects of fructose metabolism, it aids the body in maintaining healthy liver fat levels and reducing the cellular stress that leads to long-term dysfunction.
What is Fatty Liver?
Fatty liver is a buildup of fat in liver cells, often without symptoms at first. Over time, it can progress to inflammation (NASH), fibrosis, cirrhosis, and liver failure.
Causes
The most common non-alcoholic cause is fructose overconsumption, which drives liver fat synthesis via de novo lipogenesis.
The Fructose Pathway
Fructose is taken up by the liver and rapidly converted into fat, depleting energy and generating uric acid. Even without sugar, endogenous fructose production can continue the cycle.
Consequences
Fatty liver contributes to:
- Insulin resistance
- Inflammation
- Higher cholesterol
- Increased disease risk
LIV3's Role
By targeting fructose metabolism directly—with fructokinase inhibitors and uric acid reducers—we believe fatty liver can be reversed at the metabolic source, not just masked through calorie reduction."